2019 TEAMS
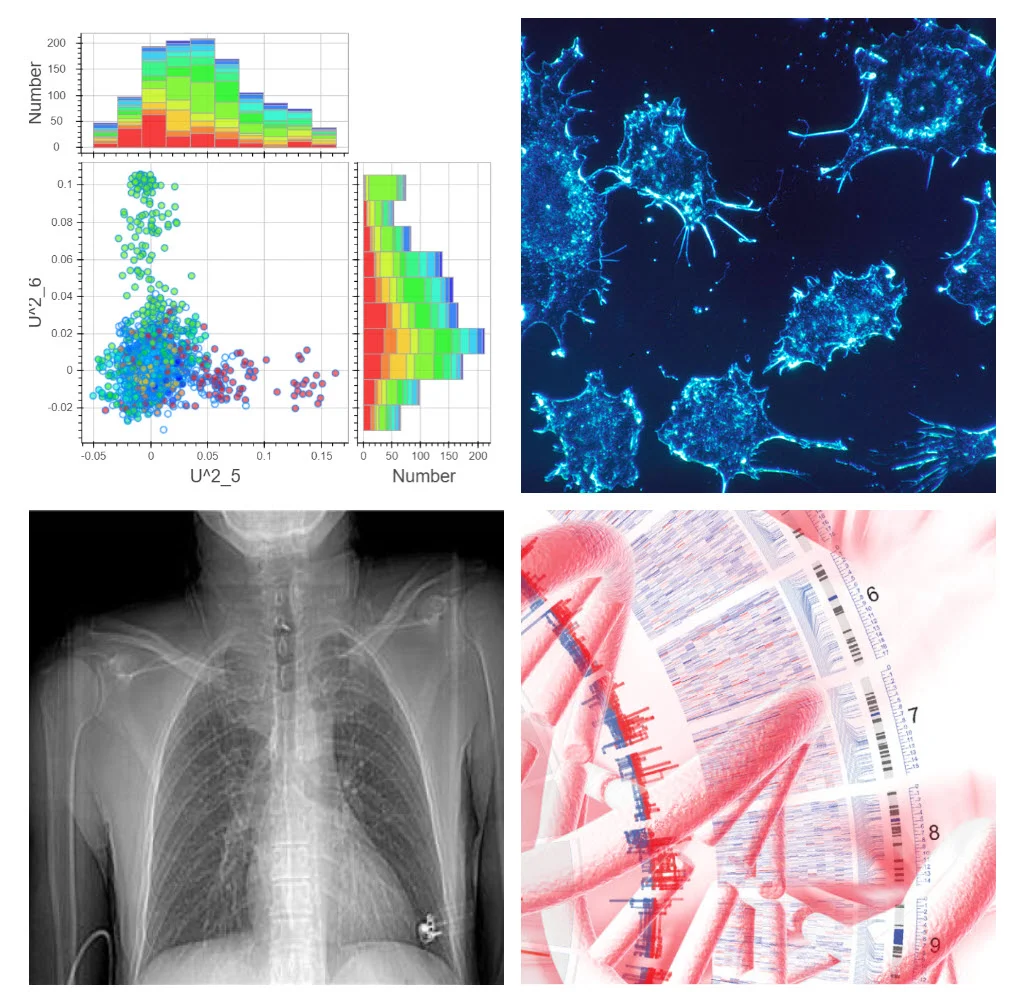
Team 7: Using Machine Learning to Improve Post-Acute Rehabilitation Process Flow
Develop a prediction model to streamline the transition of care process for hospital patients transitioning into rehabilitation facilities, with the goal of decreasing acute length of stay, facilitating outside referrals when needed and decreasing attrition from our health system.
The Centers for Medicare and Medicaid Services (CMS) require patients to have acute medical needs and intensive therapy requirements to receive care at an inpatient rehabilitation facility (IRF). Predictive models that target patients with a higher probability of IRF admission can lead to decreased length of acute hospitalization, improved bed flow and lower acute care costs. Under the approval of the United States Congress, CMS implemented the per-discharge Prospective Payment System for IRF care based on functional improvements and a patient meeting the “60% Rule” of qualifying diagnoses by primary ICD10 code.
At UTSouthwestern, admission coordinators screen potential IRF candidates for reasonable and necessary criteria, then calculate the percentage of patients who have qualifying IRF diagnoses. If the percentage does not top 60%, patients with non-qualifying diagnoses would not be admitted, even if a bed is available. This process is not only cumbersome, it is time consuming. UT Southwestern would benefit from a prediction model, which takes into account the reasonable and necessary criteria for IRF admission on the acute care service, the existing qualifying diagnoses on the IRF service and IRF bed availability for non-qualifying diagnoses.
This prediction model would streamline the transition of care process, with the goal of decreasing acute length of stay, facilitating outside referrals when needed and decreasing attrition from our health system. Should this predictive model prove successful, we could test intervention fidelity using the 2019 data. There are over 1100 IRFs in the United States, and there is no existing data on the use of machine learning to improve process flow for post-acute care. Therefore, there is a high likelihood of clinical utility for this intervention.
Team Lead: Nneka Ifejika, MD, MPH, Physical Medicine and Rehabilitation, utswmed.org/doctors/nneka-ifejika/
Team 8: Automated algorithm for detecting and localizing enteric tubes to facilitate accurate and timely radiographic interpretation
Create an image analysis tool to accurately localize enteric tubes and flag potential problems on radiographs in clinical practice.
Misplaced enteric tubes can result in significant morbidity, including pneumothorax, pleural effusion, retropharyngeal abscess and lung abscess. In clinical practice, radiographs are used to confirm position of enteric tubes. These radiographs may be reviewed by the primary team or interpreted by the radiologist prior to starting enteral feeding or medications. Although rare, missed malpositioned enteric tubes can lead to catastrophic consequences including patient death. Mistakes in interpretation can occur due to poor image quality, distracting findings on the radiographs (such as presence of other tubes or pathologies) , or consequence of other human error. An accurate algorithm automatically localizing enteric tubes can help reduce such errors. The algorithm could also flag potential positive studies on reading worklists to facilitate prioritization of interpretation by a radiologist, regardless of length of the reading queue.
We will utilize approximately 1000 abdominal radiographs without enteric tubes and about 1000 radiographs with tubes in place, and bounding box information for localization of the tips of the catheter. Our goal is to create a solution that can reliably identify whether a tube is present and pretty close at deriving bounding boxes that enclose the terminal tip of the tubes. In the final product, the locations of the terminal tips can be used to identify images containing malpositioned tubes, potentially through statistical means or cluster analysis.
Team Leads: Travis Browning, MD and Ye Seng Ng, MD, Emergency Medicine, profiles.utsouthwestern.edu/profile/42192/travis-browning.html
Team 9: Real-Time Cardiac Assessment of Catheterization-Derived Fick and CMR-Derived Flow
Improve workflow, reliability and reproduciblity of interventional cardiac MRI through a web/app-based user-friendly display for real-time assessment.
Cardiologists are tasked with the role of determining complex hemodynamic information that is important to determine the need for catheter-based and/or surgical intervention. Today’s standard of care practice involves performing cardiac catheterization and cardiac magnetic resonance (CMR) separately. Catheterization by x-ray is used primarily to collect pressure and saturation data and to intervene on hemodynamically significant holes in the heart. In addition, interventionalists are able to place stents, coils, and percutaneous valves. Meanwhile, CMR is a powerful emerging tool to help cardiologists and CT surgeons answer complex physiology questions by showing very accurate function and flow data.
Interventional cardiac magnetic resonance (iCMR) is a new approach in congenital cardiology gaining traction around the world. In the US, the National Institutes of Health (NIH) and Children’s Health Dallas are the only two centers currently actively pursuing this research in the congenital heart population. iCMR is like a normal heart catheterization, but the procedure occurs in the MRI magnet instead of the catheterization X-ray lab. It is our hope that a radiation-free heart catheterization will become standard of care for patients in the future.
We would like to improve the workflow and ease of calculating important hemodynamic information derived by cardiac catheterization, CMR, and/or iCMR. These numbers are important because they will help guide therapy and are often what surgeons and cardiologists analyze to determine if intervention is necessary. Cardiac catheterization and CMR use different techniques to ultimately produce the same hemodynamic information. Both techniques use simple but unrelated equations to determine the patient’s systemic and pulmonary cardiac flows. The current workflow of using these equations is completely manual and subject to human error.
Our goal is to improve workflow, reliability, and reproducibility by improving the accessibility of these hemodynamic equations through a web/app-based user-friendly display that will allow the operator to obtain information in real time.
Team Lead: Yousef Arar, MD, MPH, Pediatric Cardiology, www.utsouthwestern.edu/education/medical-school/departments/pediatrics/divisions/cardiology/
Team 11: Optical coherence tomography-angiography in glaucoma
Develop a deep learning tool that will parse OCTA data facilitating diagnosis of early glaucoma and its progression and that will rule out non-glaucoma conditions.
Glaucoma is the second most common cause of blindness worldwide. It is believed that glaucomatous optic neuropathy is the result of combination of mechanical stress and reduced blood supply to the optic nerve. Up till now, we have based glaucoma diagnosis and progression on the level of intra-ocular pressure (IOP), optic nerve cupping and visual field (VF) testing but these modalities have inherent weaknesses. Optical coherence tomography angiography (OCTA) is a robust, non-contact noninvasive imaging system that provides reproducible, 3-dimensional, high resolution, volumetric and quantitative data of the retinal layers including vascular networks in retina, optic nerve and choroid. Currently, there is no effective way of analyzing data from ever expanding field of OCTA including understanding the role played by age, gender, race, refractive errors, hypertension and diabetes. We propose to develop a deep learning tool that will parse OCTA data facilitating diagnosis of early glaucoma and its progression and that will rule out non-glaucoma conditions.
Team Lead: Karanjit S Kooner MD, Opthalmology, profiles.utsouthwestern.edu/profile/13996/karanjit-kooner.html








