2019 TEAMS
team 2: A Deep convolutional neural network for identifying thyroid cancer
Develop a more accurate system for identifying thyroid cancer by applying a deep convolutional neural network algorithm to data from a UTSW thyroid cancer database.
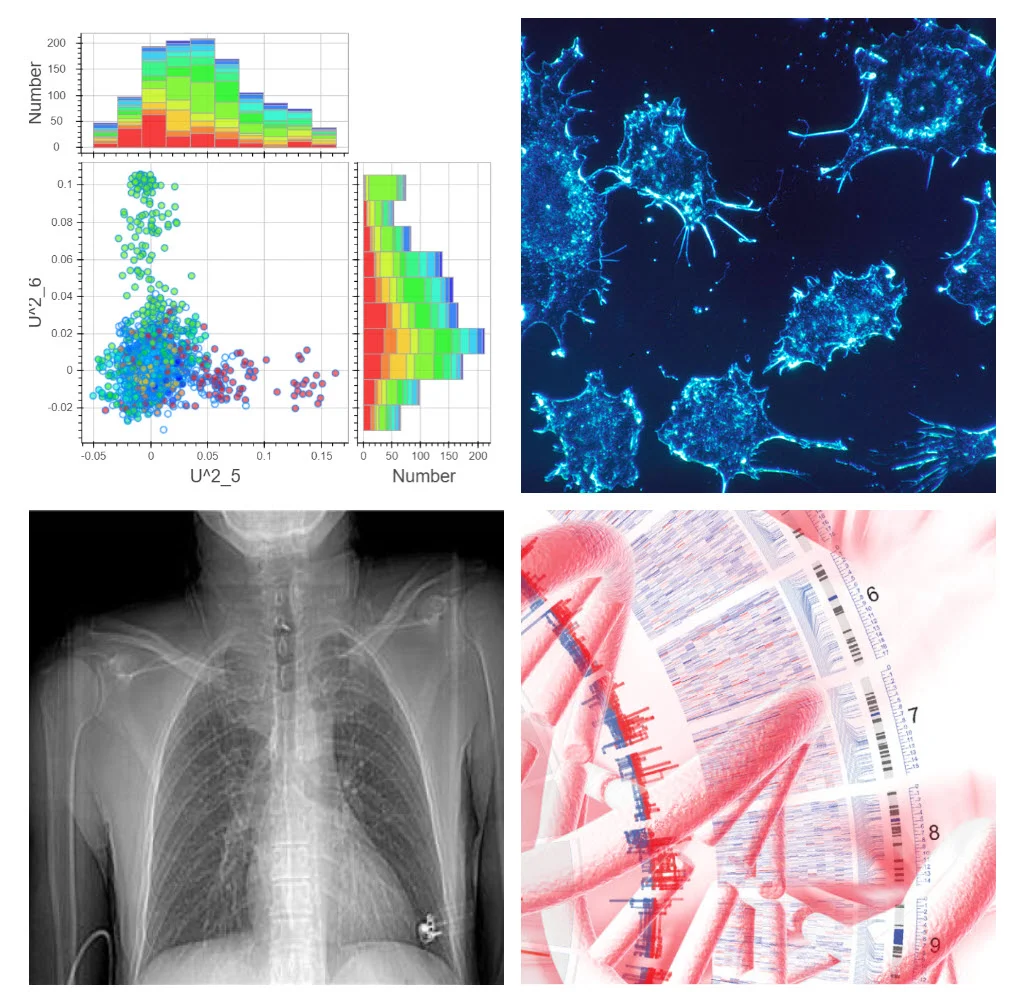
Differentiating benign thyroid nodules from cancer is a significant health challenge, as thyroid nodules are present by ultrasound (US) in a staggering 19 – 35% of the general adult population (approximately 130 million people). Most of these nodules are benign, however the diagnostic process is costly, inefficient, and leads to unnecessary surgery and morbidity. We propose to develop a more accurate system for identifying thyroid cancer by applying a deep convolutional neural network (DCNN) algorithm to data from our thyroid cancer database, which includes a large number patients who have been followed clinically for several years. We propose to develop a new risk prediction and prognosis tool to predict the individualized risk of death and recurrence from thyroid cancer. We envision two modes of analysis; 1) exploratory analysis, and 2) clinical performance optimization. In the exploratory mode we will leverage advanced unsupervised machine learning techniques such as manifold learning and dimension reduction (DR) to visualize multi-modal, integrated, high-dimensional data (as a point cloud). We hope to build an interactive, GUI-based data visualization dashboard to allow rapid traversal of this complex data by scientists and clinicians alike. Additionally, we will incorporate and overlay the proposed predictive models as they are developed and refined, and provide the ability to annotate data/models on the fly for subsequent use with other models. In the second mode, performance optimization, we will build on the recognition patterns discovered in the augmented data exploration, and then refine and optimize specific candidate predictive models emphasizing those with high potential for clinical impact/utility. The most high-performing predictive models will then be validated retrospectively and prospectively. At the conclusion of this project, we will have a deep learning tool that has improved ability to detect thyroid cancer in patients with thyroid nodules. We also anticipate that we will have a risk prediction tool that accurately identifies the risk of recurrence and death after initial treatment of thyroid cancer. Through this process, we will have established one of the first comprehensive annotated databases of thyroid ultrasound images that will allow development and validation of a deep learning algorithm to accurately differentiate benign from malignant thyroid nodules.
Team Lead: Fiemu Nwariaku, MD, Surgery, https://www.utsouthwestern.edu/labs/nwariaku/
Team 7: Using Machine Learning to Improve Post-Acute Rehabilitation Process Flow
Develop a prediction model to streamline the transition of care process for hospital patients transitioning into rehabilitation facilities, with the goal of decreasing acute length of stay, facilitating outside referrals when needed and decreasing attrition from our health system.
The Centers for Medicare and Medicaid Services (CMS) require patients to have acute medical needs and intensive therapy requirements to receive care at an inpatient rehabilitation facility (IRF). Predictive models that target patients with a higher probability of IRF admission can lead to decreased length of acute hospitalization, improved bed flow and lower acute care costs. Under the approval of the United States Congress, CMS implemented the per-discharge Prospective Payment System for IRF care based on functional improvements and a patient meeting the “60% Rule” of qualifying diagnoses by primary ICD10 code.
At UTSouthwestern, admission coordinators screen potential IRF candidates for reasonable and necessary criteria, then calculate the percentage of patients who have qualifying IRF diagnoses. If the percentage does not top 60%, patients with non-qualifying diagnoses would not be admitted, even if a bed is available. This process is not only cumbersome, it is time consuming. UT Southwestern would benefit from a prediction model, which takes into account the reasonable and necessary criteria for IRF admission on the acute care service, the existing qualifying diagnoses on the IRF service and IRF bed availability for non-qualifying diagnoses.
This prediction model would streamline the transition of care process, with the goal of decreasing acute length of stay, facilitating outside referrals when needed and decreasing attrition from our health system. Should this predictive model prove successful, we could test intervention fidelity using the 2019 data. There are over 1100 IRFs in the United States, and there is no existing data on the use of machine learning to improve process flow for post-acute care. Therefore, there is a high likelihood of clinical utility for this intervention.
Team Lead: Nneka Ifejika, MD, MPH, Physical Medicine and Rehabilitation, utswmed.org/doctors/nneka-ifejika/
Team 8: Automated algorithm for detecting and localizing enteric tubes to facilitate accurate and timely radiographic interpretation
Create an image analysis tool to accurately localize enteric tubes and flag potential problems on radiographs in clinical practice.
Misplaced enteric tubes can result in significant morbidity, including pneumothorax, pleural effusion, retropharyngeal abscess and lung abscess. In clinical practice, radiographs are used to confirm position of enteric tubes. These radiographs may be reviewed by the primary team or interpreted by the radiologist prior to starting enteral feeding or medications. Although rare, missed malpositioned enteric tubes can lead to catastrophic consequences including patient death. Mistakes in interpretation can occur due to poor image quality, distracting findings on the radiographs (such as presence of other tubes or pathologies) , or consequence of other human error. An accurate algorithm automatically localizing enteric tubes can help reduce such errors. The algorithm could also flag potential positive studies on reading worklists to facilitate prioritization of interpretation by a radiologist, regardless of length of the reading queue.
We will utilize approximately 1000 abdominal radiographs without enteric tubes and about 1000 radiographs with tubes in place, and bounding box information for localization of the tips of the catheter. Our goal is to create a solution that can reliably identify whether a tube is present and pretty close at deriving bounding boxes that enclose the terminal tip of the tubes. In the final product, the locations of the terminal tips can be used to identify images containing malpositioned tubes, potentially through statistical means or cluster analysis.
Team Leads: Travis Browning, MD and Ye Seng Ng, MD, Emergency Medicine, profiles.utsouthwestern.edu/profile/42192/travis-browning.html






